When I began researching knowledge sharing in NHS Estates and Facilities Management (EFM), it was because during the first wave of COVID-19, I had seen first-hand the intense pressures facing teams responsible for keeping our hospitals running smoothly and safely. At that time, I was volunteering at Addenbrooke's Hospital in Cambridge, where we were confronted with unprecedented numbers of COVID-19 patients requiring up to 60 litres per minute of oxygen - dramatically changing how the hospital's medical gas pipeline system was utilised compared to its original design (pictured above is me among the team of volunteering engineering students, reviewing schematic drawings of the medical gas pipeline system to determine the available infrastructure and capacity). EFM might seem invisible to many, but it underpins the very ability to deliver safe, effective healthcare. Today, these teams navigate an increasingly challenging landscape: complex, ageing infrastructure, growing maintenance backlogs, shrinking budgets, and a 300k-strong workforce stretched thin. Given these intense demands, I quickly realised improving collaboration across the NHS wasn't just a "nice-to-have" but essential, as the NHS cannot afford to make the same time-consuming and costly mistakes over and over again.
Ageing Infrastructure in Crisis
A staggering maintenance backlog of £13.8 billion has accumulated, with over half tied to buildings at significant risk of failure (1). The consequences aren't abstract. In 2021-22, NHS England reported 5,348 clinical incidents directly linked to estates and infrastructure failures, more than double the number reported in 2016-17 (2), clearly illustrating how poorly maintained and outdated facilities, compounded by a lack of investment, severely affect patient outcomes.
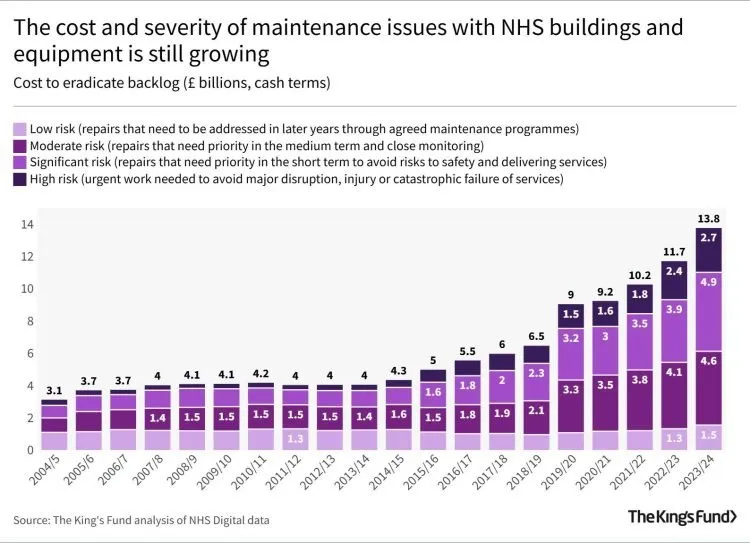
Maintenance backlog and capital investment in the NHS (in £bn) (3)
The dramatic situation is summarised by Sir Julian Hartley, chief executive of NHS Providers:
“The cost of trying to patch up creaking buildings and out-of-date facilities is rocketing. [. . . ] The safety of patients and staff is at stake. To provide first-class care the NHS needs safe, efficient and reliable buildings, facilities and equipment.” (4)
Workforce Under Pressure
About 34% NHS EFM professionals are approaching retirement age (compared to 19% of overall NHS workforce) and only 5% are under 25 (5). Hence, succession planning is a daunting task, exacerbated by an ageing workforce and challenges in attracting young professionals. During my research, I frequently talked to EFM professionals who had recently joined the NHS, reporting about their steep learning curves and the critical need for transferring tacit knowledge from experienced staff.
This means that 34% of the most experienced staff are set to retire from the NHS in the coming 10 years - representing a huge loss of practical, site-specific, and often undocumented knowledge unless urgent action is taken. However, internal knowledge-sharing practices often fall short, fragmented by organisational silos and overwhelmed by daily demands. Effective knowledge sharing isn't just about procedures and best practice documents; it’s about fostering trust, creating incentives, and developing systems that enable smooth information exchange.

Age distribution of NHS EFM workforce shows that 34% of staff are nearing retirement (5)
The Big Question: How Can We Share What Matters?
I was certainly not the only one recognising the value of leveraging the collective knowledge in the NHS:
“[. . . ] opportunity to develop the connections and sharing culture conducive to knowledge sharing, which can support the NHS in its quest to develop as a learning organisation.” (NHS, 2016)
“[. . . ] new arrangements must help overcome the barriers to productive collaboration that organisational and professional self-interest can erect.” (Lord Carter of Coles, 2016)
“[. . . ] organisations within NHS England must find ways to work together across organisational boundaries [since] it may be the only way to deliver a successful NHS” (NHS Professionals, 2019)
Looking at the challenges and previous attempts, I asked myself: how can NHS Estates and Facilities teams share the right knowledge, with the right people, at the right time, especially when so much of that knowledge risks walking out the door? That question became the focus of my PhD, which explored how knowledge is shared (or not shared) across NHS EFM departments, and what practical steps can improve it.
What’s Coming Next: Insights from the Research
In the coming blog posts, I’ll unpack the key themes that emerged from this research. I’ll start with a closer look at what types of knowledge really matter in the world of healthcare infrastructure - beyond what’s written in policies or manuals. Then I’ll explore the channels teams actually use to share knowledge - from informal networks and professional networks to national platforms such as the NHSE Collaboration Hub.
I’ll also share insights from case studies on medical oxygen infrastructure during the first wave of COVID-19, which revealed just how much was being improvised - and how much better things could be with stronger collaboration. Finally, I’ll explore the organisational, cultural, and social factors that shape knowledge flow in practice, and introduce ten NHS EFM personas from Technicians to Directors of EFM, based on interviews and questionnaires with professionals at every level of the system.
If you recognise your team in this, let me know. I'd love to hear how you’re tackling knowledge sharing on the ground.
-1.png?width=431&height=115&name=Untitled%20design%20(2)-1.png)


