In recent weeks, I explored how human resource bottlenecks limit time for reflection, collaboration and knowledge sharing among NHS EFM staff. This week, I'm diving into the organisational barriers that compound these challenges - institutional factors that participants ranked as the biggest obstacles to effective knowledge sharing.
When bureaucracy cecomes the enemy of progress and innovation
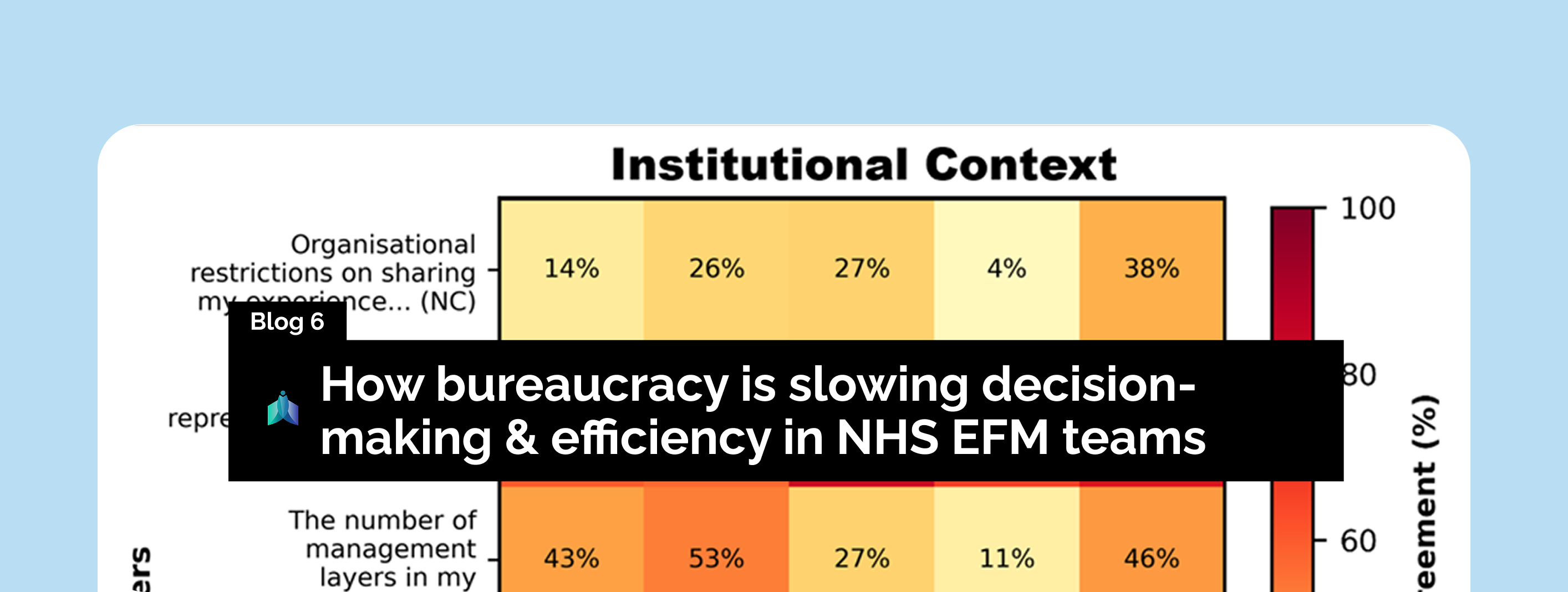
The level of NHS bureaucracy topped the list of barriers, which won't surprise anyone with public sector experience. Heads of EFM (82% agreement) and Authorising Engineers (85% agreement) felt this most acutely. In public-private partnerships, particularly PFI scenarios, bureaucracy becomes especially time-consuming. Multiple case study interviewees criticised the NHS's decision-making culture.
"Decisions on where to spend the money: dreadful, absolutely dreadful. [...] Because they're afraid of making the wrong decision".

Figure 1: Institutional Context Barriers by Job Level
This bureaucratic paralysis doesn't just slow operations. It actively prevents the visits to other sites and learning opportunities that could drive system-wide improvements.
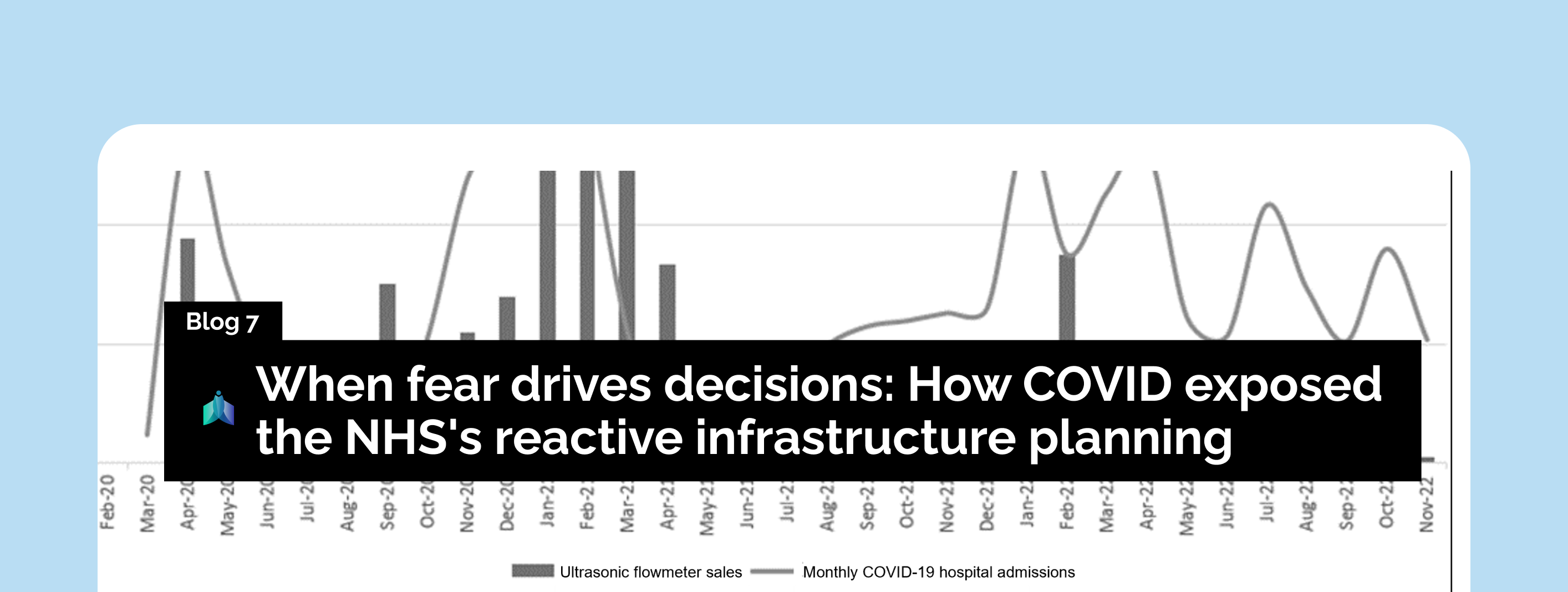
COVID proved change is possible (but quickly reversible)
The pandemic offered a glimpse of what's possible when bureaucracy steps aside. Suddenly, Trusts could act decisively: "during the pandemic, most Trusts were able to do things quickly, similar to the private sector."
An Authorised Person was "really proud" of the Trust's decisive action during the pandemic, while a Head of Estates found positives despite the chaos: "it was very difficult, there were lots of unknowns, but there were some positives in the way that we were able to carry out our service."
This streamlined approach wasn't isolated. An NHS Confederation report contrasted "the agile response to the COVID-19 pandemic in parts of London with the bureaucratic and slow-moving approach used in developing partnership working pre-pandemic."
Yet here's the frustrating part: most parts of the system immediately reverted to old ways. "It just feels the pandemic never happened and we're just back to normal ways of working," one Director of EFM lamented. This indicates a missed opportunity to embed crisis-driven efficiencies.
Missing EFM voices at the board level
Here's a telling statistic: across my seven case study Trusts, not one had a Director of EFM as an executive board member. Over 65% of Heads of EFM, Directors of EFM, and Authorising Engineers see this lack of board representation as a critical barrier.
Without direct board access, EFM perspectives struggle to influence strategic decisions. One Head of Estates highlighted the absurdity:
"Considering the costs associated with the Estate, the lack of EFM representation on the board has always been an issue. There is also a conflict of interest as our [Director of Estates] is also our Finance Director".
The reporting pathways vary wildly. Some Directors report directly to CEOs, allowing EFM voices to be heard "on equal terms to the other services." Others report through CFOs, focusing on financial and contract management (as seen in Blog 3) or via Chief Nurses, aligning with EFM's "impact on patients and the quality of [care]."
But indirect representation has real consequences. EFM issues are "sometimes not high on the board agenda." An AP put it bluntly:
"Activity challenges [...] such as cancer referral rates [...] are always going to be trumping the Estate."
When communication breaks down at every level
Even robust risk registers - essential for keeping backlog risks visible at board level - can't overcome fundamental communication failures. Interviewees described that EFM departments are "too top-heavy with managers managing managers" with "too many layers for quick decision-making."
This creates dysfunctional feedback loops. One AP described the frustration: "We escalate [and] they go to these meetings, but they don't feed back to us." Another echoed this disconnect: "from the information that comes back down, it would lead me to believe that the Estates interest isn't discussed very much at board level."
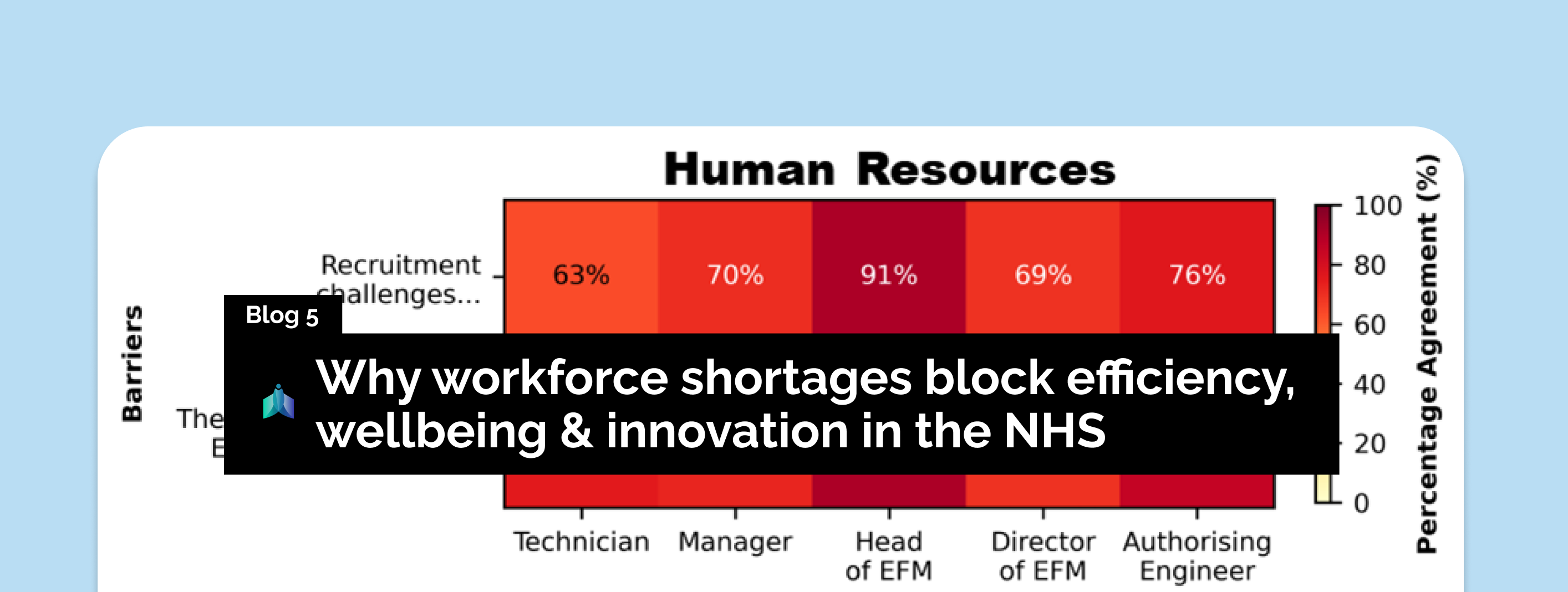
But the problem runs deeper than poor communication flows. Heads of EFM and Authorising Engineers highlighted a critical issue: senior managers often lack technical expertise (Figure 2). One Manager observed:
"It happens all the time: people taking positions without meeting the essential or desirable criteria."

Figure 2: Leadership & Management Barriers by Job Level
The lack of technical competency among senior managers creates significant barriers, with 92% of Authorising Engineers and 82% of Heads of EFM highlighting this issue. Ineffective management practices compound the problem, showing consistently high agreement across most job levels. This creates a toxic "them and us" culture, where senior management are perceived as "mostly clueless about what needs to be done in the real world."
Ultimately, this can result in technical decisions made by non-technical people who don't understand the consequences.
An AP captured this challenge perfectly:
"The Chief Exec, they don't want to know the detail, but they want you to explain it to them in a way that they understand. [...] In the end, non-technical people make technical decisions without fully understanding the repercussions [...] but the devil is in the detail [...]. That's where my job comes in to actually take it from a technical perspective."
The path forward: transparent and streamlined compliance workflows
Across NHS EFM teams, compliance management is still bogged down by admin-heavy processes. Risks are collated in multiple committees, copy-pasted into separate spreadsheets, stored locally, and updated only when someone finds the time. As a result, there is duplication, wasted effort, and blind spots. One Trust described the same risk being raised in both Infection Prevention and Control and Water Safety groups, with neither realising they were duplicating work.
These barriers are fixable. What’s needed is a single, integrated system where compliance information is visible across the organisation, supported by AI to strip out manual repetition. Done right, this isn’t just about efficiency - it frees EFM professionals to focus on reflection, collaboration, and knowledge sharing, the real drivers of improvement.
If you're interested in exploring how we can help transform your compliance workflows from bureaucratic burden to strategic advantage, reach out directly at carl@innex.ai.
Want to dig into the details? Read the full thesis here.
-1.png?width=431&height=115&name=Untitled%20design%20(2)-1.png)

.png)
