When I started researching what knowledge actually matters in NHS Estates and Facilities Management (EFM), I expected a fairly simple pattern: technicians need operational skills, managers need tactical skills, directors need strategic thinking.
That’s not what I found.
Through a Delphi study with 165 EFM professionals across all levels, I uncovered something more complex - and in some cases, more worrying. The data reveals clear mismatches between what people are expected to know, what they’re taught, and what they actually need to do their jobs well.
These aren’t just academic gaps. They affect how teams communicate risk, plan for the future, adapt to emergencies, and embrace innovation. And they’re holding the system back.
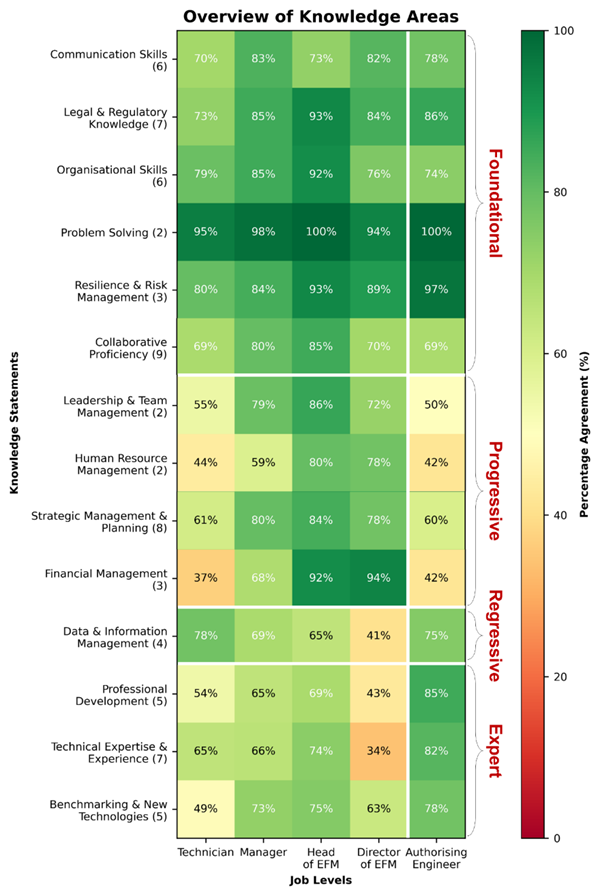
Overview of knowledge priorities across EFM managerial levels - the darker the green, the higher the percentage of professionals rating that knowledge area as very or extremely important.
Finding 1: Communication is essential but still not taught
EFM staff constantly have to translate technical risks into clear, practical terms for clinical, executive, and finance colleagues. But this vital skill isn’t part of most estates-related training.
One Head of EFM described struggling to “explain risk to the organisation” - a challenge that directly affects investment, safety, and crisis response. As another noted, communication is a “core skill of any in-house estates manager”, but still “not something taught on surveying or estates-related courses".
The technical jargon that's second nature to EFM staff becomes a barrier when they need buy-in for critical infrastructure investments. As a result, technically capable teams often struggle to get buy-in - putting trust, and patient safety, at risk.
Finding 2: The finance focus creating leadership bottlenecks
In many Trusts, EFM now reports into the Chief Financial Officer. Directors are pulled into financial oversight, while Heads of EFM are left juggling strategy, operations, and people - often without the right support.
As one Head of EFM put it: “My senior managers are not 'Estates' people - they don’t know how to use my skills.” Another noted: "Top management should be writing and setting the strategies and procedures, but this is often delegated down the ladder" to operational managers "with a trade background and mediocre technical report writing skills." In other words, the strategic functions are being pushed downward without the necessary training or capacity to deliver them well.
Managers are expected to lead in complex structures, often without being line managers, and without formal training. The leadership load is heavy - and the pipeline is fragile. As one Head of EFM asked bluntly: “Where are the next Directors and Heads of service coming from?”
Finding 3: Data is overlooked - and it's blocking digital progress
Technicians rated data management as essential (78%), but that priority drops off sharply at senior levels, with less than half of Directors considering it an important skill. This disconnect has serious consequences.
During COVID-19, several Trusts were forced to invest heavily in updating documentation. As one Head of EFM explained: "we've had problems with the drawings being wrong [...], so we invested in getting the drawings redone and made accurate." But even after such investments, gaps persist: "We put this new manifold for RSV patients in paediatrics. But there was no money in the project to update the drawings. It is absolutely mad."
Another manager pointed to the systemic nature of the problem: "so much data and duplicate data stored with no standardised folder structure." Yet the people with budget authority to fix these systems don't prioritise them.
At INNEX, we see this pattern across Trusts. Many want AI tools to magically analyse their data and deliver smart insights - predictive maintenance, risk prioritisation, automated compliance. But too often, the data is either missing or so fragmented and low-quality that even the best data analysts would struggle to make sense of it.
The result is a vicious cycle: poor documentation, weak decision-making, and stalled digital ambitions. Until senior leaders invest in the basics of data quality and structure, AI-powered data analytics in EFM will remain more hype than reality.
Finding 4: Outsourcing expertise leaves teams vulnerable
Authorising Engineers (AEs) are deeply trusted by internal teams. As one manager said, “If I had any questions or issues, I’d phone the AE up.” Another agreed: “Our first port-of-contact would be the AE.” The research underlined a clear and dangerous dependency. Areas such as Technical Expertise, Professional Development, and Benchmarking New Technologies were ranked as top priorities by AEs, but received far less attention from internal EFM staff.
This reliance comes with risk. AEs manage portfolios of 40-200 hospitals and aren’t always available, especially during crises. One AE recalled the COVID period:
“My phone didn’t stop ringing from sort of Boxing Day onwards […].” During that time, many AEs were redeployed to build Nightingale hospitals, leaving frontline teams without critical support.
That means, that many EFM teams depended on external individuals who could not always be there when it mattered most. By outsourcing so much expertise, Trusts have created a hollow core. Without internal capability to assess new technologies or sustain deep technical understanding, infrastructure resilience and the innovation capabilities suffer.
Finding 5: Sustainability is still an afterthought
Despite the NHS’s net zero commitment by 2040, Environmental & Sustainability Awareness was the only knowledge area that received no mentions in job descriptions and was not identified by participants as a priority - despite being widely emphasised in facilities management literature and NHS policy.
This is a major red flag. Post-COVID, most estates upgrades focused on resilience, not long-term efficiency. As one Head of EFM put it: “Climate change, net zero - where is the money coming from to upgrade the estate?”
This gap isn’t just about environmental impact - it’s about long-term financial sustainability. In a system already stretched, failing to invest in climate-conscious infrastructure now means greater costs and risks later. But with teams consumed by day-to-day pressures, the skills to plan for tomorrow’s resilience simply aren’t being developed. While the system is busy fighting today’s fires, tomorrow’s catastrophe is being quietly ignored.
So what?
These findings highlight a simple truth: what EFM teams are expected to do, and what they’re actually trained and supported to do, don’t always line up.
Communication, leadership, data, internal expertise, and sustainability aren’t “nice to have” - they’re core to delivering safe, efficient, and future-proof infrastructure. But they’re often underdeveloped or missing entirely from job descriptions, training programmes, and organisational priorities. To support NHS infrastructure effectively, we need to rethink how we develop people in these roles. That means training that combines communication with technical know-how, preparing Heads of Estates for complex leadership demands, treating data as a core operational asset, building internal expertise rather than outsourcing it, and making sustainability part of everyday decisions - not a side project.
At INNEX, we’re working to bridge these gaps - connecting people, knowledge, and systems so the right insights reach the right hands at the right time. Because the next crisis won’t wait for a perfect org chart or a rewritten job spec.
Want to dig into the details? Read pages 146-170 in the full thesis here.
-1.png?width=431&height=115&name=Untitled%20design%20(2)-1.png)
.png)